Abdominal Aortic Aneurysm
Abdominal Aortic Aneurysm (AAA) -- learn about causes, symptoms, treatments, and more.
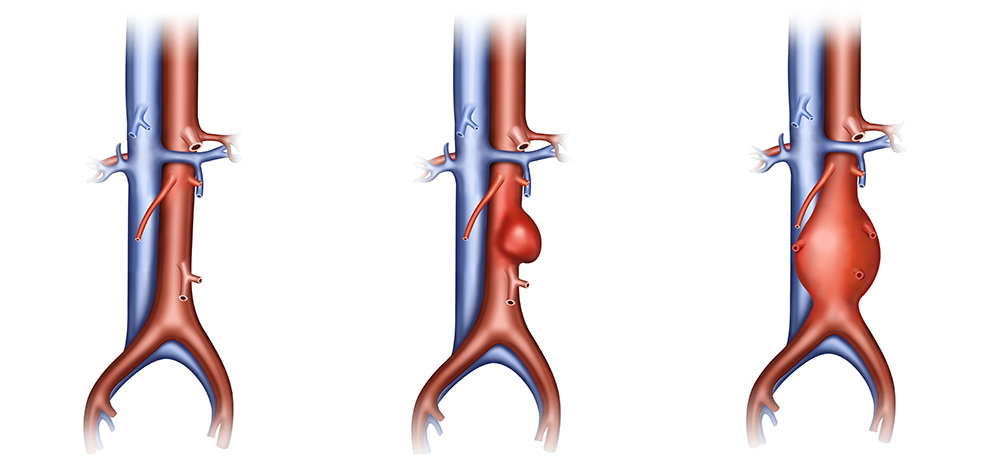
WHAT IS AN ABDOMINAL AORTIC ANEURYSM (AAA)?
The aorta is quite thick and runs directly from the heart down the center of the chest and abdomen. Because the aorta is the body’s primary method of delivering fresh blood to the body, a rupture in the abdominal aortic wall is life-threatening if not immediately treated.
The condition is somewhat common — about 200,000 people in the U.S. are diagnosed with an abdominal aortic aneurysm condition every year. As proof of the danger, ruptured aortic aneurysm is one of the leading causes of death in the U.S. (15th highest) and a leading cause of death in men age 55 and older (10th highest).
CAUSES AND RISK FACTORS FOR AAA
Potential causes and risk factors for developing AAA include:
- Family history. Aneurysms may be hereditary, making you as much as 12 times more likely to develop an abdominal aortic aneurysm if you have a first-degree relative that ever had AAA. Indeed, up to 25% of individuals treated for AAA also have a first-degree relative with AAA.
- Tobacco or nicotine use. Tobacco use (other smoking and chewing) is a major risk factor for developing abdominal aortic aneurysms. The more you do it, the greater the risk for initial development off AAA and higher your risk for aortic rupture.
- Age. Males greater than 50 years of age and women greater than 60 years of age are thought to be at a much higher risk of developing abdominal aortic aneurysms.
- Gender. Abdominal aortic aneurysms develop in males much more frequently than females.
- Trauma. Traumatic incidents (e.x., vehicle accidents) can cause an abdominal aortic aneurysm.
- Infections. Bacterial and fungal infections in the aorta may contribute to the development of abdominal aortic aneurysm.
- Inflammation and/or Vascular Disease. Inflammation and blood vessel disease in the aorta can lead to the development of AAA and increase your risk for aortic rupture.
- High blood pressure. You are at higher risk for developing AAA if you also have high blood pressure. Increased pressure on the aortic walls can weaken the aorta, leading to the development of an aneurysm.
- Atherosclerosis. You are at higher risk for developing AAA if you’ve experienced any hardening of the arteries.
SYMPTOMS OF AAA
Symptoms that may be experienced as an abdominal aortic aneurysm develops:
- Persistent, sudden, or sever back pain
- Pulsating sensation in or around the navel
- Persistent, sudden, or severe abdomen pain
Symptoms patients may experience when an abdominal aortic aneurysm ruptures:
- Sudden and severe back pain
- Sweating profusely
- Nausea and/or vomiting
- Dizziness or vertigo
- Rapid pulse
- Low blood pressure
- Pain in the back of the legs
If you experience any of the AAA rupture symptoms listed above, or you are at risk for abdominal aortic aneurysm based on a previous diagnosis by a qualified health care provider, please seek immediate medical attention.
ABOUT TESTING & WHEN YOU SHOULD GET IT
Request an abdominal ultrasound if you meet ANY of the following criteria:
- You are a male over the age of 50 with a history of tobacco use, a family history of heart disease or other vascular disease, or high blood pressure
- You are a female over the age of 60 with high blood pressure, a history of tobacco use, or a family history of heart disease, aneurysm, or sudden unexplained death
If you know you are at risk due to family history, lifestyle habits, age, etc., you should not wait to request an abdominal ultrasound. If an abdominal ultrasound detects that you DO have an abdominal aortic aneurysm you should request a referral to a vascular surgeon without delay. Vascular surgeons are specialists who are experts at managing and treating aneurysms. Your vascular surgeon will be able to give you far more detail about your condition than a general practitioner, as well as advise you regarding any additional tests needed.
NOTE: Medicare Part B (Medical Insurance) covers an abdominal aortic screening ultrasound once if you’re at risk. You’re considered at risk if you have a family history of abdominal aortic aneurysms, or you’re a man age 65-75 and have smoked at least 100 cigarettes in your lifetime.
AAA TREATMENT OPTIONS
Your vascular surgeon will choose from several different methods for repairing aneurysms and your specific diagnosis will dictate the method selected. Often times an aneurysm repair can be executed successfully using a minimally-invasive method that may only require small incisions in the groin area. Each of the methods listed below has a high success rate and Dr. Tahara can explain each to you in greater detail.
The methods available for aneurysm repair at AVV include:
Open Abdominal Surgery: This method involved the placement of a prosthetic graft and requires an incision in the abdomen. This method usually requires a hospital stay of 4 to 10 days and a total recovery time of 3 months.
Endovascular Aneurysm Repair (EVAR): This method is less invasive than open abdominal surgery and involves groin incisions. A catheter is guided in through the incisions and up to the aneurysm site. An expandable stent graft is positioned and sealed in place for permanent repair.
Regardless of the repair method selected, rest assured that Dr. Tahara and his staff give you full access to the latest technologies in vascular medicine.
Don't take risks. Get evaluated now.
CALL US at 814-368-8490 to schedule a comprehensive vascular evaluation with at AVV.