Varicose Veins
Learn about varicose veins, causes, and treatments.
WHAT ARE VARICOSE VEINS?
Varicose veins are relatively common with up to 40 million Americans experiencing the condition at some point. In fact, 40% of men and 70% of women will develop varicose veins by 60 years of age. Almost anyone can get varicose veins but women tend to develop them more frequently than do men.
CAUSES AND RISK FACTORS FOR VARICOSE VEINS
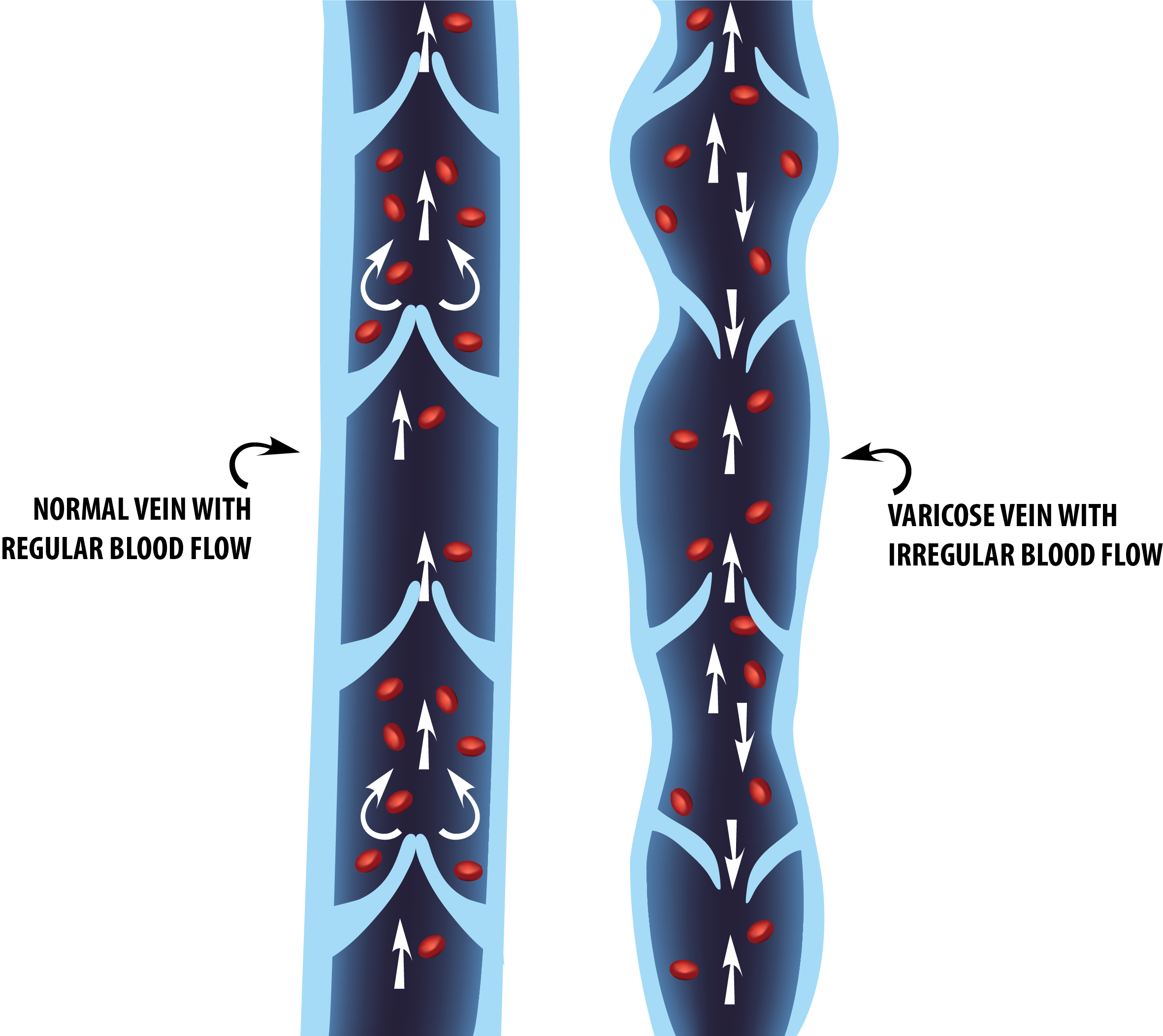
When valve failure occurs inside the veins, blood has a much harder time returning to the heart. Instead of returning to the heart, blood collects in the veins and increases pressure. Whenever veins enlarge and swell with increased pressure, varicose veins can start to form.
Potential causes and/or risk factors for varicose vein development include:
- Pregnancy. Some women experience varicose vein development while they are pregnant due to the simultaneous increase in the body’s blood volume and decrease in blood flow from the legs to the pelvic region. During pregnancy, the uterus can exert significant pressure on the veins which in turn causes those veins to enlarge. Important to note is that a varicose vein condition may improve without intervention after a time — somewhere between several months and a year after delivery. However, varicose veins may not diminish completely or much at all in some women.
- Age. Individuals greater than 50 years old are more susceptible to varicose vein development. The older we get the more elasticity we lose in our veins. Increased pressure in the veins causes them to stretch, and that subsequent stretching can weaken the veins and cause blood to flow backward.
- Gender. Varicose veins are generally more prevalent in females than males.
- Long periods of standing or sitting. The muscles in your legs and feet need to be working in order for blood to get back to the heart. Too much sitting or standing tends to increase lower extremity venous pressure over time and can lead to the gradual formation of varicose veins.
- Obesity / Overweight. Increased body weight and blood volume can increase pressure in the veins which may in turn cause varicosities to form.
- Family history. Having a family history of varicose veins is one indicator that you may be at a greater risk for their development.
SYMPTOMS
Other notable symptoms of varicose veins include:
- Pain and/or aching around the veins
- Mild to significant swelling
- Discoloration, typically below the knee
- Itchiness, burning, stinging, or throbbing
- A heaviness in the legs
- Pain gets worse after standing or sitting for awhile
- Bleeding and ulcers
Varicose veins may also clot and cause you pain. They can feel feel hot, hard to the touch, or both. We call this condition phlebitis and, though it is certainly uncomfortable, may indicate a more complex venous problem.
In the case of phlebitis, which is limited to veins closer to the surface of the skin, clots can form and it is typically not dangerous. However, any clots located within the deep veins — a condition known as deep vein thrombosis (DVT) — can be quite dangerous. Deep vein clots can break off and move to the heart or lung at any time. They pose a serious risk and usually require immediate treatment.
EXAMS AND TESTS NEEDED
The doctor may request that you have an ultrasound examination performed on your leg vein, which is typically a painless procedure that takes about 75 minutes. Ultrasound helps your vascular surgeon to identify problematic veins in both the superficial and deep venous systems so that the best treatment protocols can be selected.
VARICOSE VEIN TREATMENT OPTIONS
COMPRESSION STOCKINGS: These are socks that reach up to the knee and are designed to provide a graded compression from 20-30 mmHg with a higher compression at the the ankle than the knee, providing assistance to leg veins with poor valve function. Wearing the compression stockings properly can provide relief from aching and swelling by compressing the veins in your leg to prevent the pooling of blood. Wearing compression stockings PROPERLY is absolutely critical to the successful management of your specific vascular condition. Follow the link to learn everything you need to know about wearing compression stockings properly.
note: Please be aware that most insurance carriers do require that patients wear compression stockings for a period of no less than three months before authorizing coverage for any other varicose vein treatment options.
RADIOFREQUENCY ABLATION THERAPY: Compression stockings may prove insufficient for relieving pain and/or swelling in some individuals. If this is the case for you and certain other criteria are met (e.x., through ultrasound it is determined that veins are straight enough for treatment), ablation therapy can be an option. Radiofrequency Ablation Therapy involves the insertion of a catheter that heat seals the incompetent superficial vein, allowing blood to travel through veins that work properly. Learn more about radiofrequency ablation therapy.
VENASEAL: Learn more about venaseal.
VARITHENA: Learn more about varithena.
SCLEROTHERAPY: If the affected veins are not straight enough to accommodate a catheter used to perform ablation therapy, sclerotherapy is an option. This involves a small needle to inject sclerosant, a chemical that causes the affected veins to spasm and clot in a controlled fashion. Clots formed are not dangerous. Tiny “spider veins” can be also be treated in this manner. Learn more about sclerotherapy.
Don't let varicose veins hold you back!
Allegheny Vein & Vascular is ready to help you look and feel your best!