Endoleaks (Types I-V)
Endoleaks -- types and causes.
WHAT ARE ENDOLEAKS?
Endoleaks can occur when there is a poor seal at the proximal or distal fixation sites, or between the stent-graft components, or when there is a reflux of blood into the aneurysm sac from collateral blood vessels. Endoleaks can also occur when the stent-graft material fails and becomes porous. Endoleaks have been reported in as many as 20 to 50 percent of patients following the endovascular repair of an abdominal aortic aneurysm (AAA).
TYPES OF ENDOLEAKS
Types of endoleaks include:
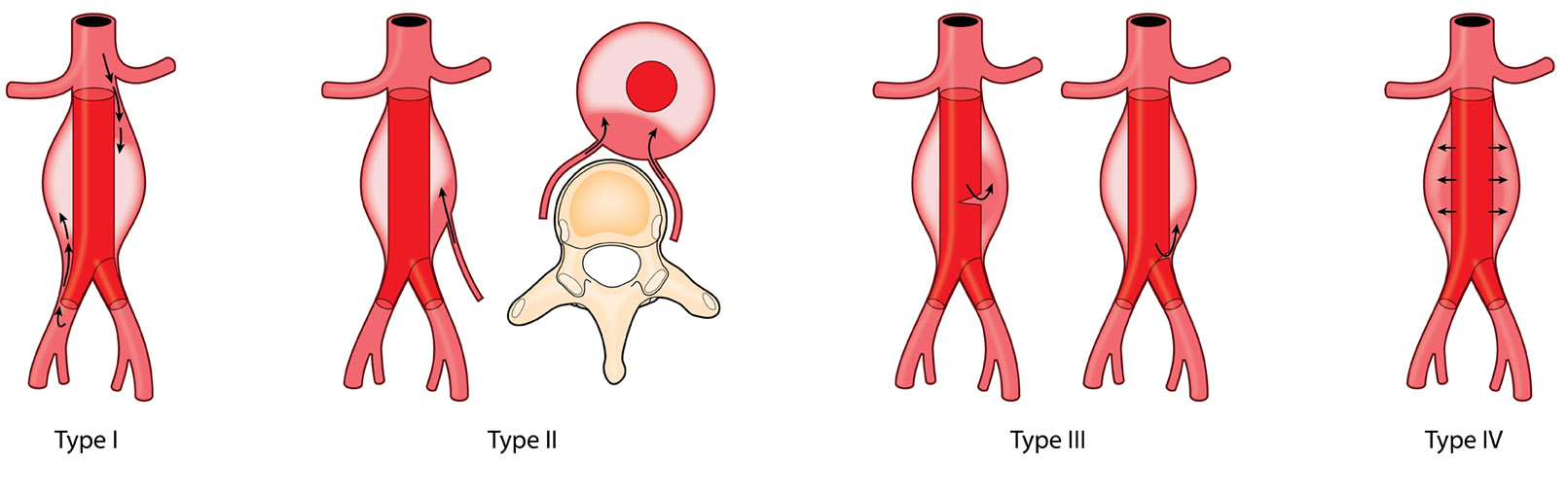
- TYPE I — this type of endoleak results from a poor seal between a stent-graft attachment site and either the native aortic or iliac arterial wall. A poor seal can cause blood to leak back into the aneurysm sac. Type I endoleaks are often immediately detected after stent-graft placement if the stent-graft does not fully dilate, or if the aortic artery is abnormally twisted (aortic tortuosity) or steeply angled. A type I endoleak can also develop later and may be related to changes in the the aorta as the aneurysm becomes smaller. Type I endoleaks are further classified by the location of the leak. Type IA endoleaks occur at the proximal aortic attachment site while type IB endoleaks occur at one of the distal iliac artery sites. Note that type I endoleaks carry a high risk of aneurysm sac rupture because the aneurysm wall is directly exposed to strong aortic pressure. For this reason, a type I endoleak must be treated with urgency.
- TYPE II — this kind of endoleak occurs when there is a reflux of blood into the aneurysm sac through collateral blood vessels such as the iliolumbar or inferior mesenteric arteries. Type II endoleaks are the most common of all types, accounting for around 40 percent of all endoleaks. Managing type II endoleaks is necessary if there is an increase in size to the aneurysm sac or when the patient presents with symptoms that could indicate sac pressurization (e.g., nonspecific abdominal or back pain).
- TYPE III — When blood leaks through the body of a stent-graft it is called a type III endoleak. This can happen when the components of a stent-graft separate or the graft material itself ruptures or tears. Just like a type I endoleak, type III is considered high-pressure and therefore high-risk. Urgent treatment is required.
- TYPE IV — A type IV endoleak is defined as leakage through the stent-graft as a result of porosity or quality of the graft material. Thankfully, this type of endoleak is less prevalent today due to modern advancements in stent-graft design and grafting material fabrication. Type IV endoleaks occur during procedures and typically resolve without intervention within 24 hours.
- TYPE V — A type V endoleak, often referred to as endotension, is where an excluded aneurysm sac continues to grow even when there is no direct radiologic evidence of a leak. The continued growth of the aneurysm sac may be caused by persistent elevation of pressure in the sac following endovascular aneurysm repair (EVAR). In the short-term, this type of endoleak is considered relatively low-risk. However, if the sac enlargement continues over a longer period then it may be necessary to intervene surgically to avoid a rupture.
TREATING ENDOLEAKS & POST-EVAR EVALUATION
Low-pressure lesions such as type II and V may be less urgent but if the aneurysm sac continues to enlarge post-EVAR, complications may arise that call for a more frequent evaluation cycle. An increase in aneurysm sac size also correlates with an increased risk for sac rupture which may eventually require treatment.
It is generally recommended that you have regular follow-up appointments with your vascular surgeon after endovascular aneurysm repair (EVAR) to monitor the size and behavior of the aneurysm sac, as well as to detect potential endoleaks. Your evaluations will involve such tests as ultrasound or contrast-enhanced angiogram (CTA). The first follow-up is usually about a month post-EVAR, then 6 months post-EVAR, and then every 6 months thereafter for the lifetime of the patient. However, Dr. Tahara will indicate the necessary follow-up schedule post-EVAR, or upon new patient evaluation and based on your unique circumstances.